My Blood Clot: Difference between revisions
mNo edit summary |
|||
| (3 intermediate revisions by the same user not shown) | |||
| Line 28: | Line 28: | ||
I noticed that the clock in my room was "nervous": the second hand would stay still for about five seconds, then it would jump forward three times, covering a total of five seconds worth of clock. Maybe I should have also paid attention to what time it was. | I noticed that the clock in my room was "nervous": the second hand would stay still for about five seconds, then it would jump forward three times, covering a total of five seconds worth of clock. Maybe I should have also paid attention to what time it was. | ||
At some point, somebody took me (together with my bed) to some place where they did ultrasounds. I guy named Steve did the [http://en.wikipedia.org/wiki/Medical_ultrasonography#Doppler_sonography ultrasound (doppler)] and found that there was some kind of blockage in my left [http://en.wikipedia.org/wiki/Subclavian_Vein subclavian vein], but that my arteries were fine, and that the right subclavian was fine. Apparently, this is a tricky area to see with ultrasound because the clavicle interferes with the ultrasound, but he could see that there was a pulse on one side (the arm side), but not on the other (the neck side), and that squeezing my arm didn't produce any flow on the neck side. I'm still looking into getting ahold of the video. Before I left, Steve told me that they would put me on some anti-coagulants ("blood thinners", which don't actually effect the viscosity of they blood). He gave me some pamphlets about [http://en.wikipedia.org/wiki/Lovenox Lovenox] and [http://en.wikipedia.org/wiki/ | At some point, somebody took me (together with my bed) to some place where they did ultrasounds. I guy named Steve did the [http://en.wikipedia.org/wiki/Medical_ultrasonography#Doppler_sonography ultrasound (doppler)] and found that there was some kind of blockage in my left [http://en.wikipedia.org/wiki/Subclavian_Vein subclavian vein], but that my arteries were fine, and that the right subclavian was fine. Apparently, this is a tricky area to see with ultrasound because the clavicle interferes with the ultrasound, but he could see that there was a pulse on one side (the arm side), but not on the other (the neck side), and that squeezing my arm didn't produce any flow on the neck side. I'm still looking into getting ahold of the video. Before I left, Steve told me that they would put me on some anti-coagulants ("blood thinners", which don't actually effect the viscosity of they blood). He gave me some pamphlets about [http://en.wikipedia.org/wiki/Lovenox Lovenox] and [http://en.wikipedia.org/wiki/Warfarin Coumadin], which I'll talk about later. He also told me that Coumadin (generic name:warfarin) was originally developed as a rat poison. | ||
I was taken back to the ER and monitored some more. A woman named Kate Landau, from vascular surgery, came to talk to me. She said that they would do a [http://en.wikipedia.org/wiki/ | I was taken back to the ER and monitored some more. A woman named Kate Landau, from vascular surgery, came to talk to me. She said that they would do a [http://en.wikipedia.org/wiki/X-ray_computed_tomography CT scan] to get a better picture of how the clot is affecting blood flow, and I signed a form to allow them to do it. A little later, Kate came back again and told me that the doctor she worked with (Ronald L. Webb) had seen this kind of thing before (most everybody I met was surprised that a healthy young guy like me had a blood clot). She said that there were two ways to handle the clot: | ||
# Take anti-coagulants for a long time (like a year), but these don't actively break up the clot, they just keep clots from forming; this approach would result in chronic swelling and discomfort (possibly forever) in my left arm. | # Take anti-coagulants for a long time (like a year), but these don't actively break up the clot, they just keep clots from forming; this approach would result in chronic swelling and discomfort (possibly forever) in my left arm. | ||
#Do a [http://en.wikipedia.org/wiki/Thrombolysis thrombolysis], whereby you deliver a chemical to the clot via a [http://en.wikipedia.org/wiki/Catheter catheter] (tube inserted into the vein) which disolves the clot (I'll talk about this later); this way, I'd probably be on the anticoagulants for less time and I wouldn't have the chronic problems, but there was a slight chance (<1%) that it could cause some bleeding in the brain, which could cause a [http://en.wikipedia.org/wiki/Stroke stroke]. | #Do a [http://en.wikipedia.org/wiki/Thrombolysis thrombolysis], whereby you deliver a chemical to the clot via a [http://en.wikipedia.org/wiki/Catheter catheter] (tube inserted into the vein) which disolves the clot (I'll talk about this later); this way, I'd probably be on the anticoagulants for less time and I wouldn't have the chronic problems, but there was a slight chance (<1%) that it could cause some bleeding in the brain, which could cause a [http://en.wikipedia.org/wiki/Stroke stroke]. | ||
| Line 52: | Line 52: | ||
<table style="width: 100%; text-align: left;" border="1" cellpadding="2" | <table style="width: 100%; text-align: left;" border="1" cellpadding="2" | ||
cellspacing="2"> | cellspacing="2"> | ||
<tr> | <tr> | ||
<td>[[File:V1,1.jpg|200px|alt="lower humerus and basilic vein"|lower humerus and basilic vein]]</td> | <td>[[File:V1,1.jpg|200px|alt="lower humerus and basilic vein"|lower humerus and basilic vein]]</td> | ||
| Line 77: | Line 76: | ||
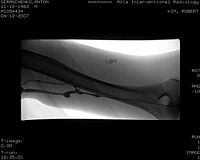
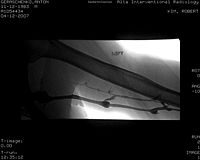
<td>Flow after three hours of TPA infusion into the clot. Its better, but still not so good</td> | <td>Flow after three hours of TPA infusion into the clot. Its better, but still not so good</td> | ||
</tr> | </tr> | ||
</table> | </table> | ||
| Line 143: | Line 141: | ||
[[Category:Blog]] | [[Category:Blog]] | ||
[[Category:My_Blood_Clot]] | |||
Latest revision as of 13:49, 16 July 2012
Short Version
I got a blood clot and had to go to the hospital for a few days. They cleared up the vein, but I'm going to have to be on anticoagulants for the next six to twelve months. This means that I'm practically hemophiliac, so I'll have to learn to avoid bleeding. In particular, I have to give up squash for a while because there is too high a chance of serious bruising. Bummer. I'm also going to have to watch my vitamin K intake.
Long Version
During my stay in the hospital, I asked lots of questions, and the nurses answered most of them. I wrote this page to have a good record of what happened to me. The purposes of this are threefold:
- it saves me some breath in explaining why I disappeared for a couple of days,
- I think some people might be curious to hear about all the details, and I don't think there is any reason to hold them back, and most importantly,
- I want to be able to look this stuff up in the future, because I know I'll forget the details.
Monday, 2007-04-09
Morning-ish I noticed that when I straightened my left arm and extended at the shoulder (as if reaching for something far away), I felt a tugging pain at the inside of my elbow, as if some connective tissue were too tight. I still don't know if this had anything to do with the clot, but I made a note of it.
I played squash with the squash team 8-10pm (as I usually did Mondays and Thursdays). A couple of times, I felt a little like I was going to black out; this kind of think would often happen when I hadn't eaten enough and I was doing some kind of heavy work. I'm pretty sure I'd eaten enough, so this was a weird event.
Tuesday, 2007-04-10
My left arm started feeling sore (as though I'd worked the muscles really hard the previous day). The hand and deltoids (shoulder) felt find, but the forearm and bicep-triceps areas got sore. My usual response to soreness is to massage the muscles to increase circulation. The arm was a little bit more red than the right arm, but I wasn't sure if this was as a result of the massaging.
Wednesday, 2007-04-11
When I woke up in the morning, my left arm was still sore, and didn't seem to have gotten better, so I called the advice nurse at the Tang Center (at around 8:30am). She said that it sounded like some sort of circulation problem and that she thought I should have it checked out at urgent care, so I had a bowel movement, grabbed my backpack, and walked down to urgent care. My blood pressure was kind of high when I got there (something like 156/95). The doctor (Anna something) there did some tests and said I might have a blood clot. After a few more tests, I had a near-faint experience; the doctor said she didn't think that had anything to do with my arm. I felt much better after some apple juice. A nurse took some vital signs; my blood pressure was lower than usual (something like 110/65), as you'd expect after a near-faint. They (nurses, I guess) took a couple of x-rays while the doctor called some vascular surgeons. They (doctor and nurses) asked if I'd had breakfast (no, I hadn't) and gave me some crackers and apple juice. Eventually, they decided to call an ambulance to take me to the ER at Alta Bates Medical Center.
Before the EMTs arrived, a nurse an IV port in my right arm (she said the ER expected me to have one). In the ambulance, the EMTs asked me some questions ("are you allergic to anything?", etc.). At the ER, they put me in my own little room (room 11). The nurse drew some blood (from the IV, which was weird; every other time they would stick me with a needle), but I don't know what it was used for. She also put some sticky rectangles on my chest which hooked up to something with monitored my pulse, respiration rate (it would start beeping when I breathed slowly), and maybe some other stuff. She also put a blood pressure cuff on me which would inflate periodically. This monitoring was pretty intensive because a bit of the clot could break off and end up in my lungs, causing a pulmonary embolism, in which case I would be in not-so-good shape. I also got a nice sign which said something like "no blood pressure or blood draw on left arm".
I noticed that the clock in my room was "nervous": the second hand would stay still for about five seconds, then it would jump forward three times, covering a total of five seconds worth of clock. Maybe I should have also paid attention to what time it was.
At some point, somebody took me (together with my bed) to some place where they did ultrasounds. I guy named Steve did the ultrasound (doppler) and found that there was some kind of blockage in my left subclavian vein, but that my arteries were fine, and that the right subclavian was fine. Apparently, this is a tricky area to see with ultrasound because the clavicle interferes with the ultrasound, but he could see that there was a pulse on one side (the arm side), but not on the other (the neck side), and that squeezing my arm didn't produce any flow on the neck side. I'm still looking into getting ahold of the video. Before I left, Steve told me that they would put me on some anti-coagulants ("blood thinners", which don't actually effect the viscosity of they blood). He gave me some pamphlets about Lovenox and Coumadin, which I'll talk about later. He also told me that Coumadin (generic name:warfarin) was originally developed as a rat poison.
I was taken back to the ER and monitored some more. A woman named Kate Landau, from vascular surgery, came to talk to me. She said that they would do a CT scan to get a better picture of how the clot is affecting blood flow, and I signed a form to allow them to do it. A little later, Kate came back again and told me that the doctor she worked with (Ronald L. Webb) had seen this kind of thing before (most everybody I met was surprised that a healthy young guy like me had a blood clot). She said that there were two ways to handle the clot:
- Take anti-coagulants for a long time (like a year), but these don't actively break up the clot, they just keep clots from forming; this approach would result in chronic swelling and discomfort (possibly forever) in my left arm.
- Do a thrombolysis, whereby you deliver a chemical to the clot via a catheter (tube inserted into the vein) which disolves the clot (I'll talk about this later); this way, I'd probably be on the anticoagulants for less time and I wouldn't have the chronic problems, but there was a slight chance (<1%) that it could cause some bleeding in the brain, which could cause a stroke.
I asked her if she could get me some more statistics. She left and came back a while later with a couple of articles and she told me that I had Paget-Schroetter syndrome (PSS). I called Lacra and asked her to find me some more articles about PSS and thrombolysis. At some point, the nurse gave me some Vicodin for the pain in my arm, but it didn't seem to have any effect.
A while later, Kate came back and told me that they weren't going to do the CT scan after all, but that they would do a venogram (I'll talk about this later), which was more accurate than a CT scan, and which would make it possible to do the thrombolysis on the spot (because the same catheter used to inject the dye for the venogram could be used to inject the chemical for the thrombolysis).
At 5 or 6, I was admitted to the hospital (taken up from the ER to a regular in-patient room), and I got a new sign ("no blood pressure or blood draw on left arm", but this one was printed, not written by hand). They took some more vital signs and took some more blood. They brought me some dinner and Lacra visited me (and brought a bunch of article about PSS and thrombolysis). Lacra and I read the articles and decided that the thrombolysis was the way to go; it was the recommended treatment in general, and I was an ideal candidate for it. We also started writing down questions about the procedures (I won't list most of the questions because the answers are in this page, on in a linked page). I think the most useful article was this one. Late in the evening, they hooked me up to a heparin IV and gave me 5mg of Coumadin. Both are anticoagulants, but the heparin starts working within a few hours, and the Coumadin takes about a week to get up to theraputic levels, so the heparin is used for that first week. If you are in the hospital for less than a week, they make give yourself Lovenox (a heparin derivative) injections until the Coumadin level is high enough. I think they also took some more blood and told me they would take more blood at 4am. I also got a new sign with said that I was on anticoagulants, so I shouldn't get injections into the muscle, and they should use small (narrow) needles for drawing blood.
Thursday, 2007-04-12
I woke up at about 3am because the other guy who was in the same room woke up. My back was really sweaty and I started shivering and couldn't stop (though I wasn't cold). I called the nurse, who took my vital signs. After I got up to go to the bathroom, I felt better and fell back asleep easily. At 4am, the nurse came to take some blood. They would take blood from me every 6 hours or so for Partial Thromboplastin Time (PTT) tests to check if I was getting the right amount of anticoagulant. The IV went through a special pump which delivered a precise amount of fluid and kept track of how much fluid was left in the bag. I think I started off getting 20mL/hr of a 50unit/mL heparin solution, but I was eventually getting 24mL/hr. She also put me on another IV of Lactated Ringer's solution. Lactated Ringer's is basically electrolytes; they put me on the IV because I wasn't going to be allowed to eat or drink anything for most of the day. I think I was getting 120mL/hr of Lactated Ringer's solution. The first vein that the nurse tried was uncooperative (it blew), but the next one was fine; now I had two IV ports (both on the right arm). I fell back asleep and woke up at around 7:30. My back was really sweaty again. The mattress was plastic under the sheat, which didn't allow any circulation of air. I had a bowel movement in the morning.
I think Kate stopped by at some point, and I asked her my list of questions, most of which she answered to my satisfaction. Around 10 or so, I was visited by Dr. Robert Kim, the interventional radiologist who would do the venogram and thrombolysis later in the day, and I asked him some more questions. Later, I was visited by Dr. Ronald Webb, and I talked to him a bit about what was going to happen and what the recovery would be like.
Around noon, I was taken to IR (interventional radiology). They put me on a table and had me lay out my left arm. Everything in the room was highly mobile: the table I was on, the x-ray machine and the monitors could all be moved around easily. I didn't actually get to see what was on the monitors because I had to lay my head back during the procedure, but I would often ask what was going on, and they would tell me.
During the first venogram, I wasn't given any sedative, just local anesthetic. Dr Kim inserted the catheter into my left arm, just above the elbow. To my surprise, having a tube run up my arm felt very much as I imagined it would. In particular, it was uncomfortable. Here are some pictures. Click on an image to enlarge it (or, in the case of flows, to see an animated gif).
 |
 |
 |
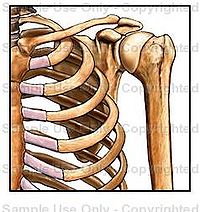 |
| My left lower humerus (upper arm). The elbow is at the far right of the picture. Some dye has been injected into my basilic vein, where they will go in with the catheter. | My upper humerus and basilic vein. | My left shoulder and rib cage. You can see the basilic vein turn into the axillary vein (which then becomes the subclavian vein). A bunch of little veins connect at that "splat". Then angle of this picture is confusing (to me). The easy-to-see parts of the ribs are actually the BACK; compare to the picture to the right. If you look carefully, you can see my left first rib. | I found the previous picture a little confusing, so here is a cartoon (taken from http://catalog.nucleusinc.com) which is a picture of almost exactly the same thing (at essentially the same angle). Note in particular how tight the curve of the first rib is. My clot was right at the pinch between the clavicle and the first rib. |
 |
 |
 |
 |
| This is the flow of blood around the clot. You can see the clavicle in the image, but the first rib is basically invisible. The two meet right where the blood stops flowing. Instead of going through the subclavian vein, the blood goes through collateral veins that take it to the same place. The fact that the collateral veins are well-developed indicates that the subclavian has been pinched for a long time. | Here you can see that the catheter has pushed through the clot. Dr. Kim said that it was tougher than he expected, indicating that the clot could have been there for up to a week. | The catheter is sticking right into the clot, and tissue plasminogen activator (TPA) is being injected into the clot. I think 4mg of TPA was injected in 2 shots of 2mg each (1mg/mL solution). | Flow after three hours of TPA infusion into the clot. Its better, but still not so good |
After injecting the clot with TPA, they hooked the catheter up to a TPA IV. A sheath went around the catheter, and a heparin IV was hooked up to the sheath. Finally, a lactated Ringer's solution IV was hooked up to my right arm. I got to talk to Dr Kim a bit after the procedure. He told me that the collateral veins could potentially become developed enough that they would completely take over the job of the subclavian vein, which sounds pretty cool to me. I was sent to recovery (where the nurse-to-patient ratio was higher than in my usual room) to be monitored while the TPA infusion was happening. My nurse was a funny woman from Thailand. At some point she brought another nurse over and said, "this is my cute patient" to which the other nurse replied, "oh, he's so cute". I asked to go to the bathroom, and she gave me a plastic jar, but I just couldn't pee while lying in bed. I tried again a little later. Eventually, she called Dr. Kim to ask if it was ok for me to stand up so that I could pee in the plastic jar. He said yes, and I was very relieved. I also called Lacra to give her an update. At around 5pm, I was taken back to IR for another venogram. I told them that my arm was feeling sore, so the nurse injected me with some fentanyl, which made me feel pretty groovy (apparently, the pain-killing potency of fentanyl is 80 times that of morphine!), though still quite alert. The flow of blood was still not so great (see the lower right picture in the above table). There was either residual clot or stenosis (where the vein itself is narrow), so Dr. Kim decided to do an angioplasty venoplasty (inflating a balloon in the vein to widen it). He used an 8mm diameter balloon, then a 10mm balloon, then a 12mm balloon. The bigger balloons didn't fit through the smaller sheath (before inflation), so he had to change to larger sheaths a couple of times, which was uncomfortable, so they gave me some more fentanyl (I think I got 150 micrograms total), and some more local anesthetic (they hit a nerve, which made the fingers of my left hand really hurt and then go numb). There was a lot of pushing stuff up and down my arm, which I would occasionally feel as pressure in my left palm, just under the middle and ring fingers.
After the venoplasty, I was feeling pretty good from the combination of fentanyl and the thought of being done with the scary stuff. I was taken back to my room and I was given some dinner and another 5mg of Coumadin. Lacra came to visit, but we couldn't think of much to talk about (also, the other guy who was in the same room was watching TV, which was very distracting), so we watched some Simpsons on the TV. As the fentanyl wore off, my left arm started hurting more. The nurse gave me some Vicodin for it (I'm not sure what the dosage was; it was a pretty big pill), but it didn't do much. I'll have to remember that Vicodin doesn't work well for me. Little muscles in my left forearm would occationally twitch a little, and at some point I noticed my left thumb twich a bit. The part of my arm between my armpit and elbow (where they had run the catheter) hurt, but the muscles weren't feeling sore anymore. My nurse gave me an ice pack which I put under my arm for the night. That helped the pain a lot.
Friday, 2007-04-13
I slept better than the first night. I still woke up at around 6am with my back all sweaty. I was given breakfast in the morning. I think I spent most of the morning reading The Blind Watchmaker. I got to talk to Kate again and tell her how things were going. When they brought me lunch, the lunch plate had a little lid on it, and for the heck of it, I decided to try picking it up with my left hand. To my irritation, the lid would twist out of my fingers and fall. Most of my hand was pretty much at full strength, but I couldn't bend my left thumb at the joint with any force at all. I called my mom and told her what was going on, then I told her about stacks and moduli problems. Later I got a call from my older brother (Peter) and we talked about stuff. After I'd spewed out all the medical terms I'd learned, Peter pointed out to me that I should make a record of what happened, because I'm going to forget the details. In particular, he told me that I should be able to get ahold of the stuff from my ultrasound and venograms. I was allowed to walk around the hospital, so I asked for a new IV pole because my old one had terrible wheels. The new one was quite a bit better, but still not very smooth. I walked around the hospital a little bit. I went to the desk on the floor and asked my nurse if I she could give me a stress ball, so that I could work the strength back into my thumb. I also asked her how I could get pictures and reports from the ultrasound and venograms. She said she'd look into it. Eventually, I was given two stress balls. It was really hard to squeeze them with my thumb; it almost felt like I couldn't even TRY to squeeze them. Lacra visited in the evening. We watched some TV and played Magic (which we hadn't done in a while). I was given 10mg of Coudamin (twice as much as the previous two nights).
Saturday, 2007-04-14
Shortly after midnight, I had some blood taken. The nurse brought a box for me, which contained a booklet about Lovenox, and a red plastic jar, where I could throw out the needles. I slept quite well, but again my back was very sweaty in the morning. After breakfast, I was visited by Dr. Webb. He said that it looked like the vein was still in not such great shape. The venoplasty stretched the vein out, but it still is quite tight. This means that I will probably have chronic swelling in my left arm, and that I'll have to be on Coumadin for a while. In Dr. Webb's experiance, the aniicoagulants help the collateral veins to develop. I asked him if there is some kind of physical therapy I can do to help them develop better, and in general to help reduce the amount of uncomfortable swelling in the future. He said that he didn't usually have patients do physical therapy unless they'd had a surgury, but I was quite perssitant, saying that there has to be something I can focus on. I felt like he avoided the issue a bit, saying that it's something that would be better for us to talk about when we meet in two weeks to check up on things. I reminded him to write some orders for them to release the venogram pictures to me. After he left, I got up to walk around the hospital. I talked to the charge nurse, and told her about my unsatisfying conversation about physical therapy. She made a note in my chart that I'm interested in physical therapy. I went to the first floor of the hospital (my room was 6513A, on the sixth floor) and wandered around. I found myself in radiology and figured I'd ask about how to get ahold of my venogram pictures and reports. I filled out some papers in the radiology records office. The woman there said that the pictures were there, but that the reports weren't transcribed yet, so I'd have to get them later, but that I could pick up a CD with the pictures as soon as I was discharged. I also asked about the ultrasound, but she couldn't find any record of it; it must have happened in some other department. I found the general office of medical records, but it was closed, so I'll have to look for the ultrasound later.
At about 2:30, Lacra came over and my nurse showed me how to stick myself with Lovenox. I was surprised that sticking the needle in didn't hurt very much. What stings is injecting the stuff. Also surprising to me was that there was no bleeding after I removed the needle (it goes into the skin where my love-handles should be). The nurse also brought me a CD with the venogram pictures (which are in the tables above). After that, I was discharged, and Lacra and I went home.
Then we went to the Tang Center to get my perscriptions. The Tang Center pharmacy said that they didn't have Lovenox or Coumadin, so I'd have to get it elsewhere. Lacra and I walked to the Long's Drugs on Shattack, but they didn't have Lovenox either. The Walgreens in downtown Berkeley did have Lovenox and Coumadin. Six syringes of Lovenox cost $495! This kind of irritates me because when you get a perscription from the Tang Center, you pay something like $15 no matter what it is (SHIP covers the rest), but when you go to another pharmacy, you only get reimbursed 70%.
I ran into a friend of mine in downtown Berkeley and brought him home for dinner, which was very nice.
Sunday, 2007-04-15
I wrote this web page. It was also my first day sticking myself with Lovenox (once in the morning and once in the evening).