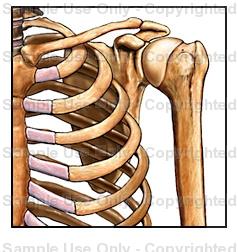
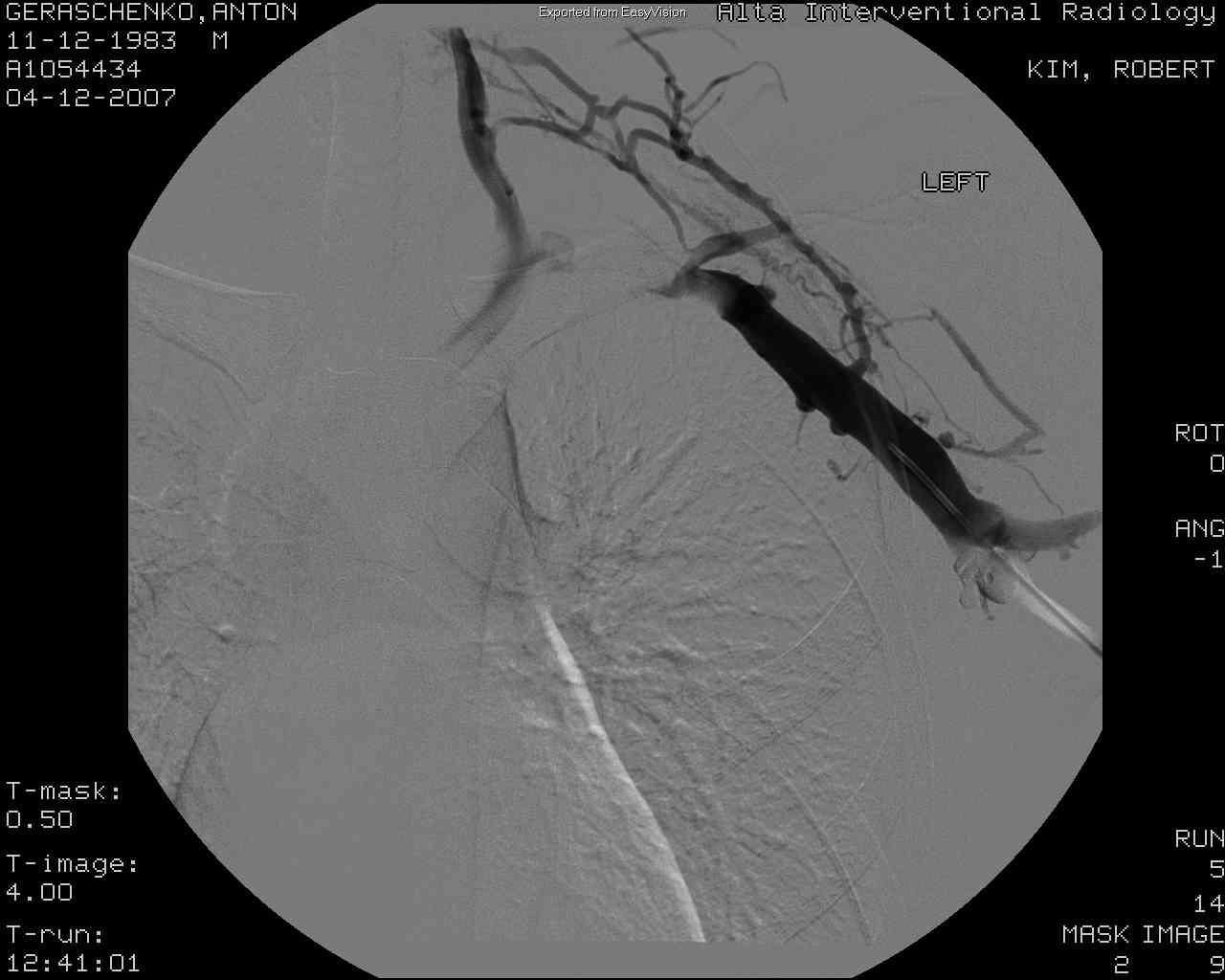
My left lower
humerus (upper arm). The elbow is at the far right of the picture. Some
dye has been injected into my basilic vein, where they will go in with
the catheter.
|
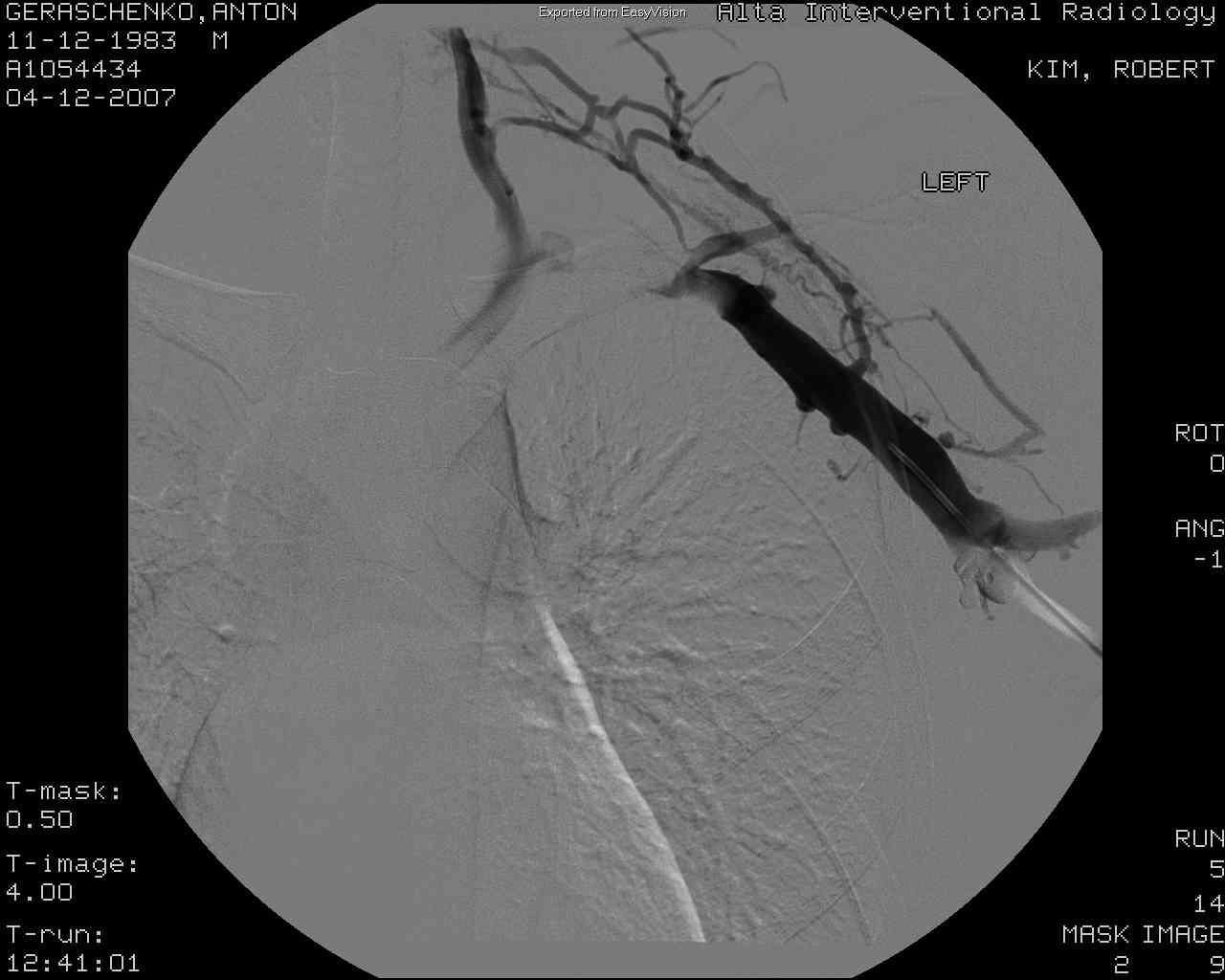
My upper humerus and basilic
vein.
|
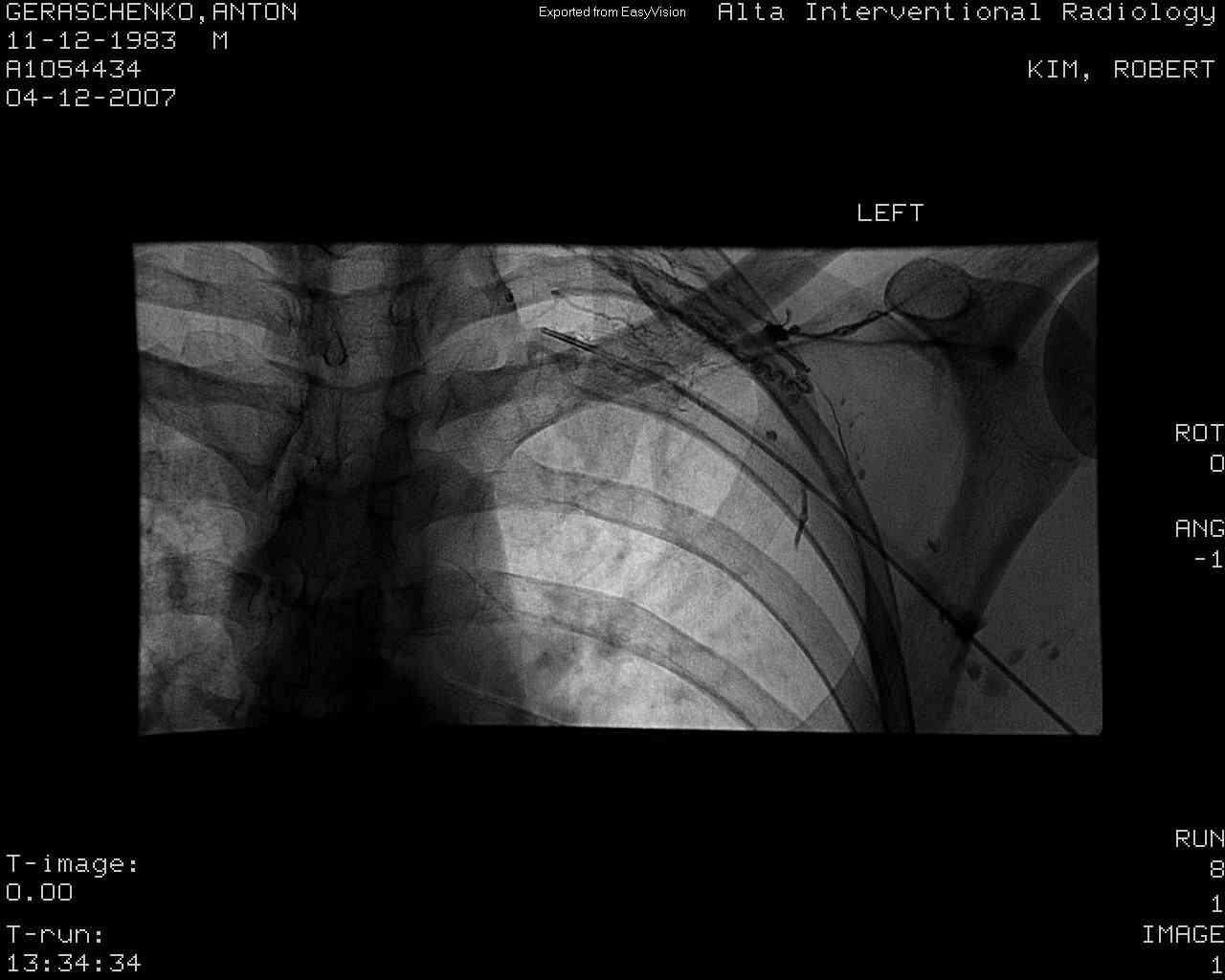
My left shoulder and rib cage.
You can see the basilic vein turn into the subclavian vein. A bunch of
little veins connect at that "splat". Then angle of this picture is
confusing (to me). The easy-to-see parts of the ribs are actually the
BACK; compare to the picture to the right. If you look carefully, you
can see my left first rib.
|
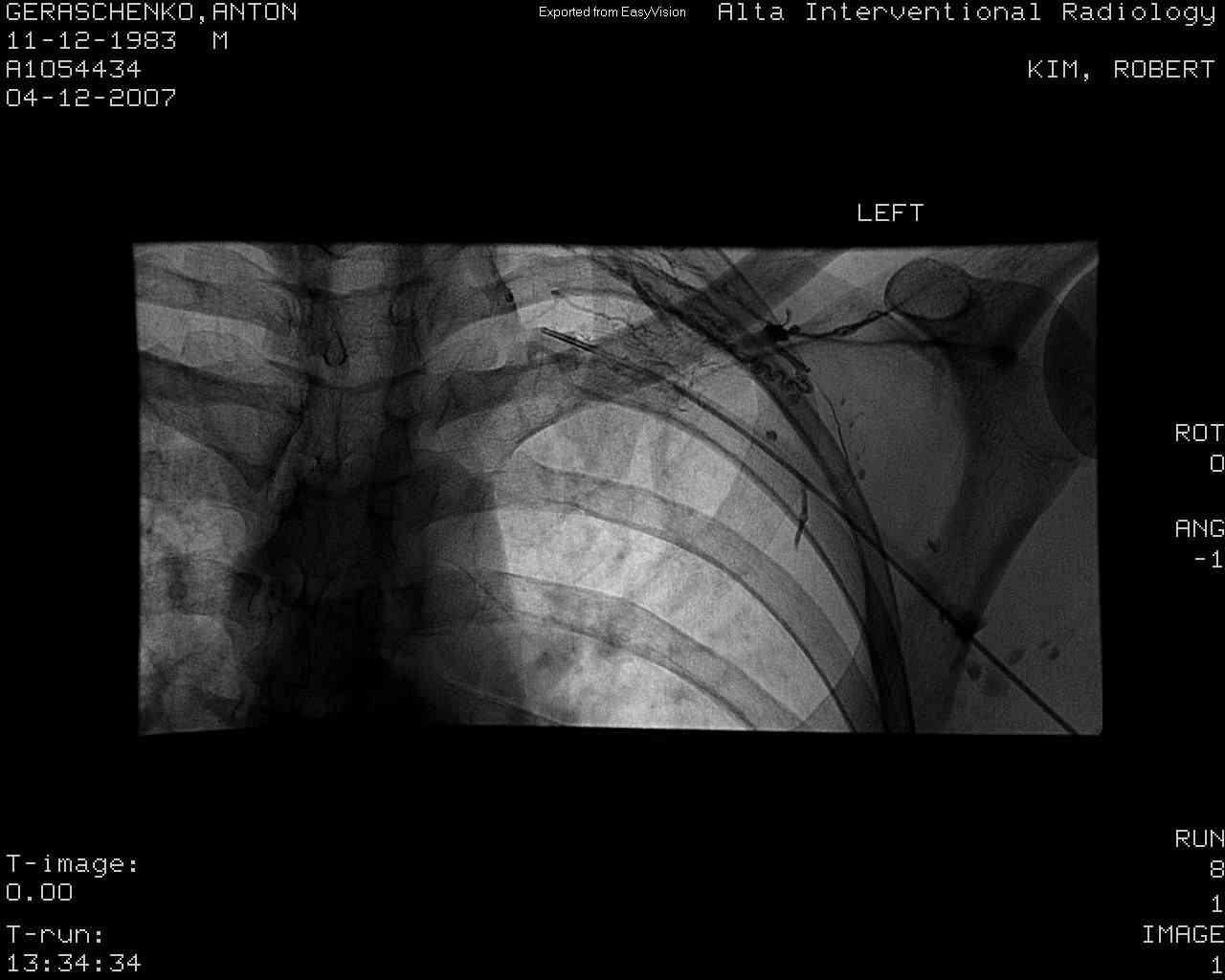
I found the previous picture a
little confusing, so here is a cartoon (taken from http://catalog.nucleusinc.com)
which is a picture of almost exactly the same thing (at essentially the
same angle). Note in particular how tight the curve of the first rib
is. My clot was right at the pinch between the clavicle and the first
rib.
|
| This is the flow of blood around
the clot. You can see the clavicle in the image, but the first rib is
basically invisible. The two meet right where the blood stops flowing.
Instead of going through the subclavian vein, the blood goes through
collateral veins that take it to the same place. The fact that the
collateral veins are well-developed indicates that the subclavian has
been pinched for a long time. |
Here you can see that the
catheter has pushed through the clot. Dr. Kim said that it was tougher
than he expected, indicating that the clot could have been there for up
to a week. |
The catheter is sticking right
into the clot, and tissue
plasminogen activator (TPA) is being injected into the clot. I
think 4mg of TPA was injected in 2 shots of 2mg each (1mg/mL solution). |
Flow after three hours of TPA
infusion into the clot. Its better, but still not so good |